This week I was at St. Joseph’s Candler Hospital for my rotation in the Diabetes Management Center (DMC). I had a pretty good week here, and I learned a lot about diabetes from the two RDs in the DMC, Aggie and Windsome. On Monday, Meagan and I learned how to take blood sugar. We also did rounds with Windsome, one of the RDs in the DMC (who is also a registered nurse and certified diabetes educator). She taught us how to fill out a card before going up to see the patients and explaining what was relevant to us. We then were assigned to go to the Wellness Center in the afternoon. We learned about a diabetes program and that was really it. There was way too much down time and thankfully we didn’t spend more time down there. However, we did have to go to a class that talked about diabetes in relation to Periodontal Disease. It was taught by dental hygiene students. I didn’t realize how much the mouth could be an indicator of so many diseases, so I thought it was really interesting how high blood sugars could impact the mouth so much.
On Tuesday we spent some time with Aggie learning lots about insulin pumps and how to inject insulin. I had no idea about insulin pumps and only understood the basics of how they worked so it was interesting to learn about them.
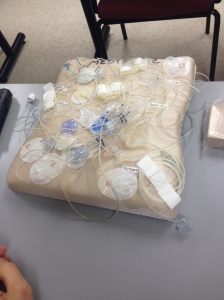
We learned how to attach them and how they worked. I can’t imagine having to do that every day, but if you want to manage your diabetes well you have to. There’s so many different pump options it’s crazy!

Learning how to pull insulin into the syringe.
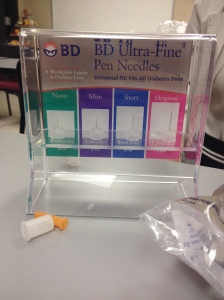
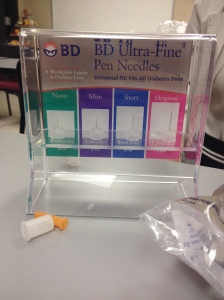
Different needle sizes.
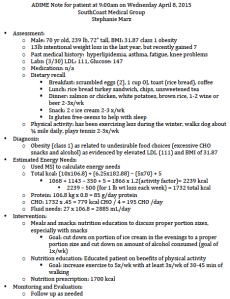
We also got to sit in on a consult of a woman who went into diabetic ketoacidosis (DKA) the week before. She wasn’t really trusting her pump and over the course of this week I have learned that is something that you have to do. DKA is caused by the breakdown of fat for energy (which causes ketones) when the blood sugar gets high and is unable to get into the cells for energy. When that happens your cells think they are starving so they start breaking down fat which leads to ketosis. This is super dangerous and can lead to death. Later, we got to do inpatient rounds with Windsome. We saw two patients, both older males, who were resistant to learning about insulin injections. One guy had had diabetes for years and though he had been giving himself insulin properly. After watching him draw up the insulin he needed in the syringe, we realized that he wasn’t drawing up the right amount, because he had a harder time reading the numbers. Unfortunately, his insurance will not cover the insulin pens (probably more friendly to older patients), so he has to use the insulin syringes. This is apparently a common sad reality among diabetes patients. He thought he was doing fine with the syringes but all this time he may not have been giving himself the proper amount of insulin. The next patient was a man recently diagnosed. He got really frustrated when Windsome told him that he was going to need to have a schedule for administering his insulin. He got defensive and tried to tell her it wasn’t going to happen and his wife was trying to calm him down. Windsome suggested that if administering two different insulins (one rapid acting and one slow release) didn’t work for him then he should try a 70/30 insulin, which is a combo insulin so you only have to stick yourself twice per day instead of four to six times per day. The downfall of that insulin is that it doesn’t give you as much control over amounts, but it is better for people that may not be compliant otherwise. After the patients we then learned how to document in the computer charting system. We also got to sit in on a diabetes education class. It went over basics and diet. It’s amazing how many of the participants had had diabetes for so many years but never received formal education about diabetes. There are so many misconceptions that people have about diabetes and what is and isn’t good to eat.
On Wednesday I was supposed to have my resting metabolic rate (RMR) measured. This is where you are fasted and are hooked up to a mask and breathe normal. I started mine and then they forgot about me so I never actually got my results, but I now know what it feels like to have one done.

Being hooked up to an RMR mask.
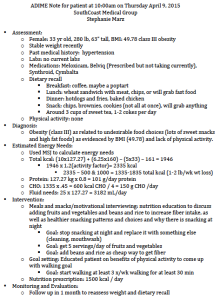
I then got to sit in on an new patient session, which is where patients get a one on one session prior to taking the diabetes classes and their specific concerns are addressed. I was amazed at one woman who has been passed around from doctor to doctor and had a couple ER visits and nobody had done anything to help her. One woman was pregnant and had some diabetes issues going on. Later in the day we made calls to patients in the program to check on their goals and see if they had been trying to meet them.
Thursday was a slower day that the others, but we still were able to see patients on the floor. We saw a couple people recently diagnosed with type 2 diabetes. One of the ladies had a big problem with drinking sugar drinks and snacking on hard candies. There was another lady who came into the ER because she ended up with polyurina and polydypsia and when the nurse at her worked checked her sugars they were over 500. Since she was so thirsty she kept drinking more and more tea (not realizing that would keep increasing her sugars). We talked to her about some basic food changes and showed her how to check her blood sugars. She is going to do the diabetes class here where she will learn more information. We also got to see a 22 year old type 1 diabetic (since she was 7!) for uncontrolled sugars. She wasn’t checking her sugars regularly so they got out of control. She also wasn’t eating properly and was skipping meals so we talked about some options for her, which included Boost for diabetics if she wasn’t willing to eat (because she also has gastroparesis).
Overall I got some good exposure to diabetes.